In the vast landscape of dental anomalies, dens invaginatus is a captivating enigma, a unique quirk in the journey of tooth development. As dental professionals, we must navigate this intricate territory with precision and care as we strive to understand and address this condition’s challenges. In this blog post, we delve into dens invaginatus, exploring its origins, manifestations, and the professional insights that guide its management. If you or a loved one has dens invaginatus, we encourage you to keep reading to learn more.
What Is Dens Invaginatus?
Dens invaginatus, colloquially termed “dens in dente” or “tooth within a tooth,” remains a subject of ongoing study within the dental community. In essence, it’s a developmental malformation where an infolding of the enamel organ during tooth formation plunges deep into the underlying dentin, creating a hidden channel or tunnel within the tooth. Imagine a microscopic spelunking expedition traversing a labyrinthine passage carved within the heart of a tooth.
The definitive cause remains undetermined, with hypotheses suggesting potential genetic predispositions or external influences during the critical phases of tooth bud development.
A profound understanding of tooth development is essential to comprehend the intricate nature of dens invaginatus. The journey from bud to cap to bell unfolds with remarkable precision under normal circumstances. However, any aberration in this complex process can give rise to anomalies, with dens invaginatus being a distinctive deviation that demands astute observation by dental professionals.
Recognizing the Subtle Indicators and Diagnosing Dens Invaginatus
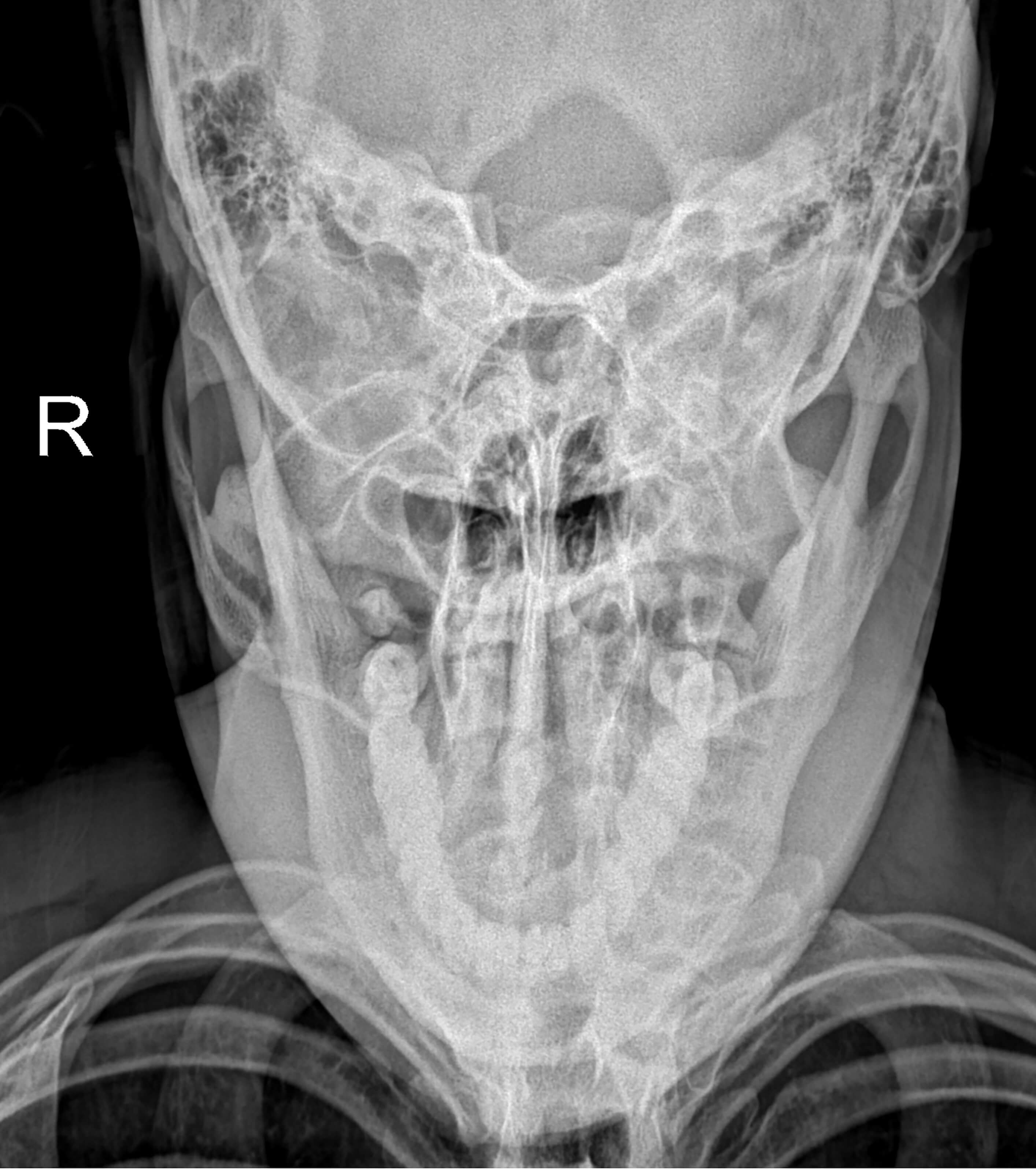
Diagnosing dens invaginatus requires keen observation, as the condition often reveals itself through inconspicuous or seemingly insignificant pits or fissures on the tooth’s surface. This subtle presentation conceals a more profound complexity, necessitating advanced diagnostic tools such as radiographic imaging.
Think of a standard X-ray as a two-dimensional detective picture. While it may not unveil the full 3D maze of a deep invagination, it can offer vital clues. Like a narrow burrow cut through the dentin, a telltale radiolucent line is often the first sign of dens invaginatus. The depth of this line, its proximity to the vulnerable pulp chamber, and any branching patterns can provide valuable insights into the severity and potential risks of the anomaly.
But for a truly comprehensive map, advanced imaging techniques like cone-beam computed tomography (CBCT) take center stage. Imagine CBCT as a 3D topographical map of the tooth, meticulously constructed from multiple X-ray slices taken from different angles. This detailed map allows us to visualize the invagination’s intricate pathways and pinpoint its exact location within the dentin and its relationship to the sensitive pulp chamber. With this precise information, dentists can confidently diagnose the anomaly, determine the best course of action, and prevent potential complications before they arise.
Types of Dens Invaginatus
There are several ways to classify dens invaginatus, but the most common and clinically relevant system is the Oehlers classification, which is based on the depth and complexity of the invagination.
The types of dens invaginatus include:
-
Type I: This is the mildest form, where the invagination is limited to the crown of the tooth. It doesn’t extend beyond the cementoenamel junction (CEJ) and doesn’t usually involve the pulp. Think of it as a shallow groove on the enamel surface.
-
Type II: This type extends deeper into the root, beyond the CEJ, but remains within the dentin. It can be a simple tunnel or branch into multiple channels. Sometimes, it may reach the pulp chamber, but it doesn’t communicate with the periodontal ligament (PDL).
-
Type III: This is a more severe form where the invagination completely penetrates the root and communicates with the PDL. There are two subtypes:
-
IIIa: This type doesn’t involve the pulp but forms a separate opening on the side of the root. Think of it as a tunnel reaching the periodontal ligament without touching the pulp.
-
IIIb: This is the most severe form, where the invagination communicates with the PDL through the apical foramen, the natural opening at the root tip. It’s like a tunnel completely bypassing the pulp and opening directly into the surrounding bone.
-
-
Type IV: This is a rare variation where the invagination not only reaches the PDL but also directly communicates with the pulp chamber. It’s like a tunnel that connects the crown, pulp chamber, and periodontal ligament.
Understanding these types is crucial for dentists as it helps determine the potential risks, treatment options, and prognosis for each patient with dens invaginatus.
Beyond the Oehlers classification, there are other ways to categorize dens invaginatus based on its shape, branching patterns, and relationship to specific tooth structures. However, the Oehlers system provides a clear and practical framework for clinical management.
Treatment Options
Dens invaginatus isn't a one-size-fits-all anomaly. Its diverse presentations demand a nuanced approach to management, where the ideal path lies somewhere between conservative preservation and definitive interventions. However, determining which course to take is a delicate dance that requires risk assessment, patient considerations, and a deep understanding of the hidden depths within the tooth.
Several factors act as guideposts on this journey:
-
Depth and Severity: The Oehlers classification serves as our compass. Mild Type I invaginations might only require close monitoring, while deeper Type III and IV presentations necessitate more proactive measures to prevent pulp involvement and infection.
-
Patient Age: Preserving pulp vitality takes center stage for children with immature teeth. Minimally invasive techniques like sealants or preventive resin restorations have become our weapons of choice. Adults with fully formed roots and potentially compromised pulp might require root canal therapy or even extraction in severe cases.
-
Overall Oral Health: A patient's existing dental condition plays a crucial role. Conservative approaches might suffice in mouths with good hygiene and minimal caries risk. Conversely, teeth already riddled with decay or existing restorations might necessitate more definitive interventions to avoid further complications.
Treatment options for dens invaginatus include:
-
Preventive Measures: For mild invaginations, sealants act as shields, blocking debris and bacteria from colonizing the hidden depths. Regular monitoring ensures timely intervention if the anomaly progresses.
-
Restorative Interventions: Deeper invaginations might call for fillings or crowns. These protective barriers seal the opening, preventing food entrapment and potential infection.
-
Endodontic Therapy: Root canals are necessary when the pulp is inflamed or infected. This procedure removes the source of the problem and preserves the tooth structure.
-
Surgical Intervention: In rare cases, complex invaginations with extensive root damage or inaccessible openings might necessitate surgical techniques like apicoectomy or flap surgery to ensure thorough cleaning and disinfection.
-
Extraction: While always a last resort, severely compromised teeth with extensive invaginations and unrecoverable pulp damage might require extraction to prevent further complications and protect adjacent teeth.
Conclusion
Dens invaginatus, with its diverse types and intricate nuances, serves as a compelling reminder that understanding tooth development deformities is an ongoing challenge within the professional realm of dentistry. If you have this condition, we encourage you to contact your dentist. Together, you can come up with a management plan to preserve your smile and ensure optimal oral health.