Your gums, the underappreciated yet essential guardians of your smile, silently shield your teeth from harm. But just like any dedicated protector, they have weaknesses. They’re vulnerable to threats like gingivitis, a mild form of gum disease that silently creeps up on millions of people worldwide. While often reversible with prompt action, understanding the culprits behind gingivitis empowers you to protect your oral health and maintain gum health.
Demystifying Gingivitis
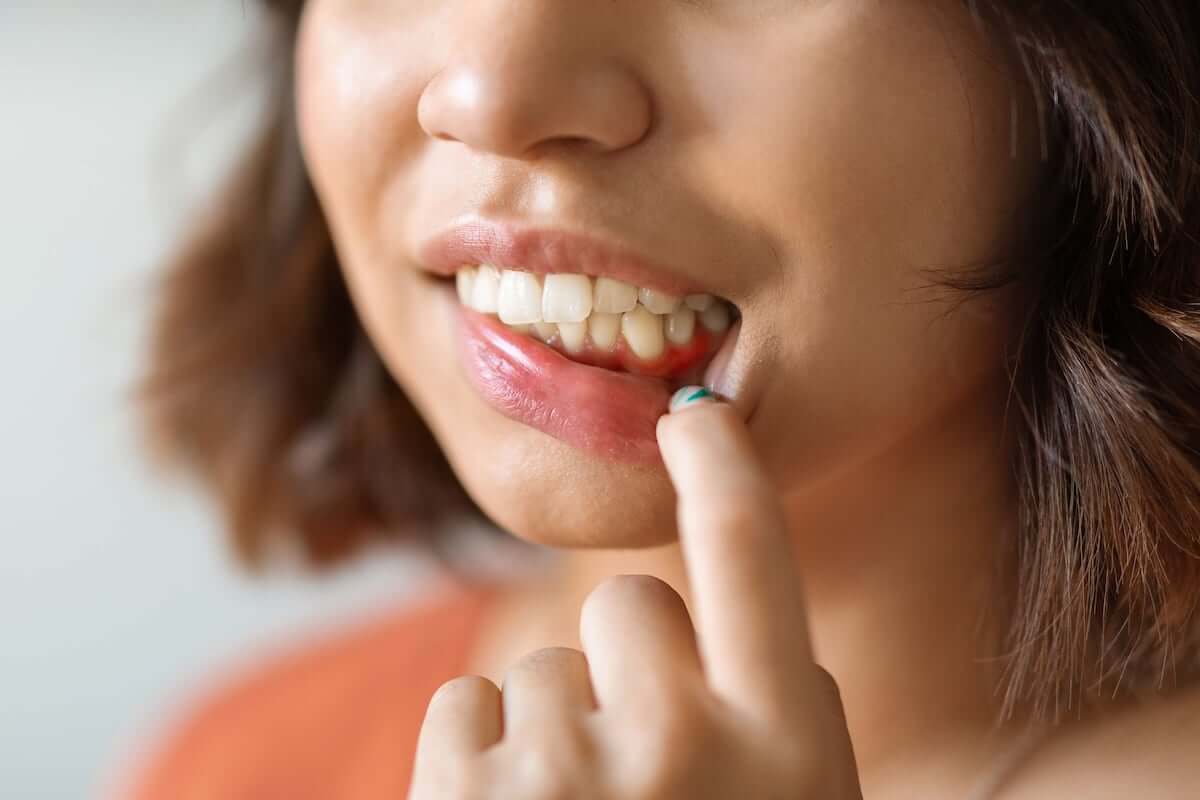
Think of gingivitis as a subtle red flag. It manifests through symptoms like redness, swelling, and occasional bleeding gums, which are often dismissed as minor inconveniences. However, left unchecked, this inflammation can evolve into periodontitis, a severe gum disease that not only compromises your smile but also impacts your overall health.
The good news?
Early detection and intervention are your allies in the battle against gingivitis and periodontitis. You can effectively prevent and manage this condition by understanding the causes of gingivitis.
The Primary Culprit: Poor Oral Hygiene
Poor oral hygiene is your arch-nemesis in the fight against gingivitis. The invisible enemy here is plaque, a sticky film of bacteria that constantly forms on your teeth. If not removed regularly through consistent brushing and flossing, plaque hardens into tartar that only your dentist can remove. This buildup irritates your gums, triggering the inflammatory response we know as gingivitis.
So, how do you outsmart this cunning adversary?
Mastering the art of proper brushing and flossing is the first — and most important — step. Brush twice daily for two minutes, meticulously reaching all tooth surfaces and employing the right technique. Remember, it’s not about vigorous strokes. Use controlled, targeted movements to effectively dislodge plaque.
Don’t neglect your gums! Gently massage them while brushing to stimulate blood flow and promote healing. Flossing once a day tackles those hidden areas between teeth where plaque loves to lurk, and rinsing with mouthwash helps get rid of anything you might miss. Remember, consistency and technique are key. It’s not just about how often you brush, but how effectively you do it.
Other Causes of Gingivitis
While poor oral hygiene is the most common cause of gingivitis, it isn’t the only one.
Other causes of gingivitis include:
-
Dietary choices: Sugary and acidic foods are essentially treats for the plaque bacteria, fueling their growth and inflammatory potential. Moderating sugary treats and incorporating fruits and vegetables rich in vitamins and minerals boosts your gum’s natural defenses. Think of it as nourishing your smile from within.
-
Smoking: This habit weakens your immune system, making it harder for your body to fight off gum infections. Quitting smoking is a victory for your lungs and your oral health. It’s a win-win!
-
Hormonal fluctuations: Pregnancy and menopause can increase your susceptibility to gingivitis due to hormonal shifts. Regular dental checkups during these periods are particularly important, as early intervention can prevent issues from escalating.
-
Medications: Certain medicines can cause dry mouth and reduce the natural cleansing effect of saliva to create an environment where plaque thrives. Talk to your physicial about other options if dry mouth is a concern. Communicating with your healthcare team is vital for maintaining optimal oral health.
-
Medical conditions: Underlying health issues like diabetes and HIV/AIDS can compromise your immune system and increase the risk of gum disease.
-
Genetics: While not the sole determinant, research suggests a potential genetic predisposition to gingivitis in some individuals. Knowing your family history can help you be extra vigilant about oral hygiene and regular dental care.
Recognizing the Signs of Gingivitis
Your gums communicate and will let you know when something is wrong. The key is paying attention to the subtle messages your gums send you.
The often-subtle symptoms of gingivitis include:
-
Bleeding gums, even during gentle brushing or flossing: Your gums shouldn’t bleed when you brush or floss. This is a clear sign that something’s amiss. Pay attention to even occasional instances of bleeding.
-
Redness, swelling, or tenderness in your gums: Visual cues like these shouldn’t be ignored. Consider them red flags urging you to seek professional help.
-
Receding gums: Do your gums appear to be shrinking, exposing more of your teeth? If so, it could be a sign of advanced gingivitis. See your dentist to stop the process.
-
Persistent bad breath: While halitosis can have various causes, persistent bad breath is a common symptom of gingivitis.
Don’t ignore even the most subtle signs of oral health problems! Schedule a dental appointment as soon as possible if you experience any of these symptoms. Early diagnosis and intervention can prevent worsening gum disease, saving you from potential discomfort, tooth loss, and even systemic health complications down the line. Remember that your dentist is your partner in maintaining your oral health, and early communication can make a world of difference.
Preventing Gingivitis
By now, you know what to do if you think you might have gingivitis. However, preventing it is your best bet when it comes to maintaining your oral health. Here are some key tactics to keep your smile healthy and vibrant.
-
Maintain a consistent and thorough oral hygiene routine: This includes brushing with a soft brush twice daily for two minutes with proper technique, flossing once a day to reach between teeth, and using a mouthwash formulated for gum health. Remember, consistency is key.
-
Schedule regular dental checkups: Don’t wait for symptoms to appear! Regular dental checkups, typically every six months, allow your dentist to detect early signs of gingivitis and intervene before it progresses. Think of it as preventive maintenance for your smile, ensuring potential issues are caught early and addressed effectively.
-
Talk to your doctor about medications: If you’re taking medications that cause dry mouth, discuss alternative options with your doctor. Dry mouth can contribute to plaque buildup, so addressing this concern is crucial for maintaining gum health.
Closing Thoughts
Taking charge of your oral health empowers you to prevent and manage gingivitis. Healthy gums are the foundation for a confident smile, fresh breath, and overall well-being. So, brush aside plaque, embrace healthy habits, and keep your smile shining its brightest.